The Importance of Healthcare Payment Integrity
What is Healthcare Payment Integrity?
Healthcare payment integrity refers to the accuracy, efficiency, and compliance of the payment process within the healthcare industry. It encompasses the various activities and strategies aimed at preventing fraud, waste, and abuse, as well as addressing billing errors and inefficient claims processing. Achieving payment integrity involves implementing measures to validate the accuracy of claims, detect fraudulent activities, and ensure appropriate reimbursement.
Ensuring payment integrity is a collaborative effort involving payers, healthcare providers, and other stakeholders in the ecosystem. By maintaining payment integrity programs, payers can safeguard financial resources and ensure healthcare dollars are utilized appropriately, benefiting both the payer and the patients.
Why Payment Integrity is Essential for Payers
Payment integrity is of paramount importance for health plans, serving as a critical safeguard against financial losses arising from fraudulent activities, billing errors, and inefficient claims processing. It plays a pivotal role in healthcare cost containment, aiding in the accurate assessment of claims and the prevention of overpayments or inappropriate payments. This proactive approach allows payers to manage costs efficiently, especially in an environment where healthcare expenses are on a continuous upward trajectory.
In addition, payment integrity enhances trust and transparency between payers and healthcare providers. By implementing robust processes and technologies to validate claims, payers can build credibility and foster stronger relationships with providers. Efficient payment processes and accurate reimbursement also contribute to provider satisfaction, reducing administrative burdens and streamlining operations.
Challenges in Maintaining Payment Integrity
Fraud, Waste, and Abuse
One of the significant challenges in maintaining payment integrity is combating fraud, waste, and abuse within the healthcare system.
These activities can have a detrimental impact on payers and lead to significant financial losses. Payers employ various strategies to address these issues such as implementing advanced data analytics and predictive modeling techniques to identify suspicious patterns and anomalies in claims data. By leveraging these technologies, payers can detect and prevent fraudulent activities and safeguard the integrity of their payment systems.
Billing Errors and Inaccurate Claims
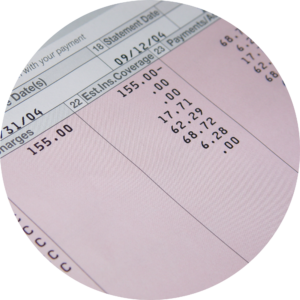 Another challenge in maintaining payment integrity is the occurrence of billing errors and inaccurate claims. These errors can arise due to coding mistakes, documentation discrepancies, or misunderstandings of reimbursement guidelines. Inaccurate claims can result in overpayment or underpayment of healthcare providers, leading to financial inaccuracies and disputes.
Another challenge in maintaining payment integrity is the occurrence of billing errors and inaccurate claims. These errors can arise due to coding mistakes, documentation discrepancies, or misunderstandings of reimbursement guidelines. Inaccurate claims can result in overpayment or underpayment of healthcare providers, leading to financial inaccuracies and disputes.
To address this challenge, payers implement robust healthcare claims auditing processes. These processes involve reviewing claims for accuracy, compliance, and adherence to reimbursement policies. By conducting regular audits, payers can identify and rectify billing errors and ensure payments are made accurately and fairly.
Inefficiencies in Claims Processing
Inefficiencies in claims processing can pose a significant challenge to payment integrity. Manual and paper-based processes, lack of standardized protocols, and complex reimbursement systems can contribute to delays, errors, and increased administrative costs. These inefficiencies not only impact payment accuracy but also affect the overall efficiency and effectiveness of the healthcare payment ecosystem.
Payers are addressing challenges by embracing robotic process automation (RPA) and artificial intelligence (AI). RPA automates repetitive tasks, reducing errors, while AI analyzes claims data to optimize processing workflows. The integration of these technologies, alongside effective auditing processes, is crucial for upholding payment integrity and sustaining a healthy healthcare payment ecosystem
Strategies for Achieving Payment Integrity
To ensure healthcare payment integrity, payers employ various strategies and technologies to identify and prevent fraud, waste, and abuse, as well as reduce billing errors and inefficiencies in claims processing. Here are four key strategies that play a vital role in achieving payment integrity:
Advanced Data Analytics

Advanced data analytics is a powerful tool in the quest for payment integrity. By leveraging large volumes of healthcare data, payers can detect patterns, anomalies, and potential instances of fraud or billing errors. Through sophisticated algorithms and statistical models, payers can analyze claims data to identify unusual billing patterns, high-risk providers, and suspicious activities.
Data analytics also enables payers to gain insights into cost containment strategies and optimize payment accuracy. By uncovering trends and patterns, payers can proactively identify areas of improvement and implement targeted interventions to enhance the overall efficiency of claims processing.
Predictive Modeling and Machine Learning
Predictive modeling and machine learning are invaluable tools in predicting and preventing potential payment integrity issues. By training models on historical claims data, payers can develop algorithms that identify patterns, predict outliers, and flag claims likely to be fraudulent or inaccurate. These models continuously learn and adapt to new data, improving their accuracy over time.
Machine learning algorithms can also assist in automating the claims auditing process, saving time and resources. By employing algorithms to review claims, payers can prioritize audits based on the likelihood of errors or fraud and ensure a more efficient and targeted approach.
Artificial Intelligence and Automation
Artificial intelligence (AI) and automation are revolutionizing the healthcare industry, including payment integrity. AI algorithms can analyze vast amounts of data quickly and accurately, identifying patterns and anomalies that may indicate fraud, waste, and abuse. By automating routine and repetitive tasks, AI-powered systems can enhance the efficiency of claims processing and reduce the risk of human error.
One of the significant advantages of AI and automation in payment integrity is their ability to continuously learn and improve. These technologies can adapt to changing trends and new fraud patterns, making them highly effective in detecting suspicious activities. By incorporating AI and automation into payment processes, payers can enhance their ability to identify and prevent fraudulent claims and ensure accurate and compliant payments.
Provider Education and Collaboration
Provider education and collaboration are essential components of achieving payment integrity. By fostering open lines of communication and providing educational resources, payers can help providers understand the complexities of billing and coding regulations. This collaboration encourages accurate claims submissions, reduces overall errors, and improves reimbursement outcomes.
Payers can offer training programs, webinars, and documentation to educate providers on coding guidelines, documentation requirements, and common billing errors to avoid. By working together, payers and providers can align their efforts to ensure accurate claims submissions and minimize payment integrity issues.
The Benefits of Payment Integrity
Cost Savings

One of the primary benefits of payment integrity is the potential for substantial cost savings. By identifying and preventing fraudulent claims, billing errors, and wasteful practices, payers can significantly reduce unnecessary healthcare expenditures by 8%-10% or more. This ensures resources are allocated efficiently and funds are directed towards providing high-quality care to patients who truly need it.
According to a study conducted by the National Health Care Anti-Fraud Association, healthcare fraud alone costs the United States tens of billions of dollars each year. By leveraging advanced data analytics, predictive modeling, and other technologies, payers can proactively detect and prevent fraudulent activities leading to significant financial savings.
Improved Compliance
Payment integrity initiatives also contribute to improved compliance with regulatory guidelines and industry standards. By ensuring claims and billing practices adhere to established rules and regulations, payers minimize the risk of non-compliance penalties and legal repercussions.
When payment integrity is prioritized, payers can implement robust processes and systems to monitor and validate claims for accuracy, appropriateness, and adherence to coding and documentation guidelines. This not only reduces the likelihood of improper payments but also enhances the overall integrity and transparency of the healthcare payment system.
Enhanced Provider-Payer Relationships
Conclusion
The benefits of payment integrity extend beyond cost savings and compliance. By embracing payment integrity initiatives and leveraging advanced technologies, payers can foster a more efficient, transparent, and sustainable healthcare system. For more insights on payment integrity in healthcare, please contact us and speak with our Payment Integrity Consulting Group.



