The Future of Medicare:
Advancing Interoperability and Streamlining Prior Authorization
Executive Summary:
We delve into the evolving and intersecting landscapes of prior authorization and healthcare interoperability for payers. Amidst increasing scrutiny related to AI-enabled denial decisions, CMS continues to waver on prior authorization rulings. We urge payers to stay ahead, navigating regulatory changes, optimizing workflows through automation, and investing in interoperability for enhanced trust and efficiency in the healthcare ecosystem.
Prior authorization (PA) has been in the news a lot lately. And more often than not, the coverage has been unflattering.
The cost-saving measure that helps plans save on unnecessary care has come under scrutiny. Partially due to the government’s slow-moving regulation process regarding PA—more on that in a moment.

However, the most damning coverage has been about Medicare Advantage (MA) plans using AI to deny coverage.
Of course, the use of algorithms in itself is not a problem. When used carefully, we think automation can improve authorization processes for plans and patients. The problem is that investigations of the denials found widespread issues and inconsistencies.
Given these headlines, payers need to be especially confident and mindful of how they proceed with their updates and messaging around PA. Of course, compliance is always important, but heightened media scrutiny increases the pressure.
At Curate Partners, we’re used to guiding our payer clients through business transformations for a variety of strategic reasons—regulatory compliance included. In this evolving regulatory landscape, we want to ensure payers stay up to date with best practices around making the most of the latest regulatory moves.
Today, we’re diving into what payers need to know about the future of Medicare policy, including:
- A timeline of recent CMS rulemaking regarding PA
- A check-in on how payers fit into the healthcare interoperability landscape
- Action steps for payers ready to level-up their PA processes and interoperability
What is the new CMS rule on prior authorization?
Prior authorization is increasingly common. A KFF analysis of Medicare Advantage plans found 35 million requests in 2021 alone.
Over the past few years, the federal government has been studying and ruling on the future of PA. They’ve been doing the same with healthcare interoperability. We wouldn’t blame you if the slew of PA and interoperability rulings from the past few years have made your head spin.
A timeline of the latest CMS moves regarding Prior Authorization and/or interoperability:

- May 2020 CMS Interoperability and Patient Access Final Rule: This rulerequired certain payers to give patients direct electronic access to their own
claims and encounter data through astandardized portal—aPatient Access API. - December 2020 Interoperability and Prior Authorization ProposedRule(Withdrawn): Building on the policies in the previous rule, this proposed rule emphasized the need to improve health information exchange. This rulespecifically focused on improving PA processes through technology.
- December 2022 Advancing Interoperability and Improving Prior AuthorizationProcesses Proposed Rule: The proposed rule emphasizes CMS’ continued commitment to increasing efficiency while keeping health information point of care availability as a central priority. The rule emphasizes leveraging FHIR standards for improved interoperability.
- April 2023 CY 2024 Medicare Advantage Final Rule: This rule prohibits MA plans from denying patients care they would otherwise receive under a traditional Medicare plan. It also required PA validity to be upheld throughout an entire course of treatment and a 90-day transition period if a patient switches to a new MA plan.
Policymakers hope that the proposed and final regulation will shorten PA wait times for Medicare Advantage, Medicaid managed care, and Affordable Care Act exchange plan patients. They also hope to quell tension regarding Medicare Advantage and traditional Medicare patients receiving different standards of care due to PA.
In the meantime, several states have passed or proposed legislation to give providers “gold cards” to bypass prior authorization. Statements by figures like Surgeon General Vivek Murthy blame PA for provider burden, adding pressure to get the rule finalized.
What payers can anticipate from CMS on these issues soon:
Another CMS move on the horizon is the expected 2024 release of the HHS Medicare managed care organization compliance audits. The Office of Inspector General (OIG) has conducted audits regarding denials of requested care that required PA.
We’re also awaiting rulemaking regarding MA plans’ use of algorithms to reject PA requests. In Congress, House Democrats are especially pushing for further regulation specifically regarding this issue.
The Ecosystem: Payers’ role in healthcare interoperability
 As intended, electronic PA intends to improve patients’ access to care, keeping the flow of information moving between facilities, payers, and patients.
As intended, electronic PA intends to improve patients’ access to care, keeping the flow of information moving between facilities, payers, and patients.
The ideal of interoperability is similar—it evokes an ethos of a harmonious healthcare ecosystem. In this ideal, providers and payers each equitably share data—and health information is always available when it’s needed, where it’s needed.
In reality, there’s a bit more friction. These delineated payer and provider roles have blurred as payer-provider relationships grow closer with more emphasis on value-based care. And communication between different sources of health data has improved with HL7 and FHIR standards—but there is still room for improvement.
The CMS requirement for a patient access, provider access, and payer-to-payer APIs and metrics reporting increases the urgency for payer interoperability improvements. But there’s a long way to go.
While payers have made great strides with ADT and CCDA data ingestion, FHIR data exchange is still “in its infancy,” per Gartner’s 2Q23 research report on U.S. Healthcare Payer Interoperability Benchmarks.
Of course, in a competitive payer marketplace, working toward interoperability is not just about compliance. It’s about providing greater value to providers and retaining a high-quality network.
What are the benefits of automating Prior Authorization?
In case you missed it, read our primer on automation technologies for healthcare payers.
Despite the challenges in these early forays into PA automation, we still see opportunity in pursuing these innovations. PA will benefit from automation—especially given the requirements around PA status reporting in the FHIR API.
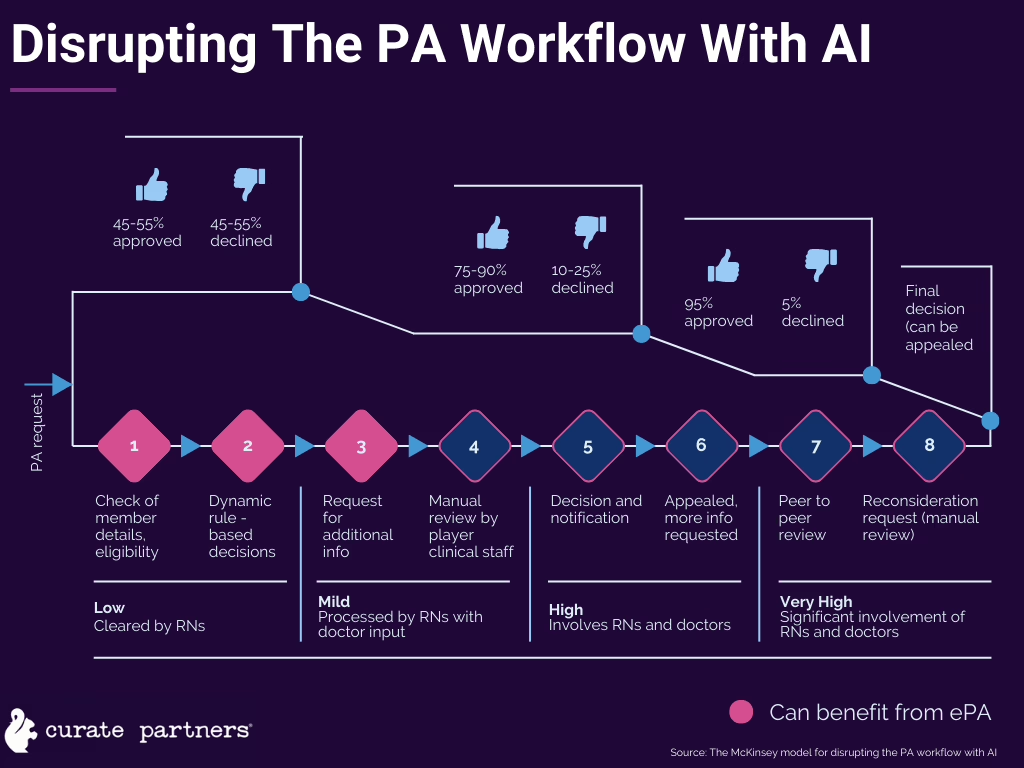
The typical PA workflow is ripe for disruption with AI-enabled automation. Per McKinsey’s analysis, we foresee the most AI disruption along the initial three steps of the eight-step standard PA workflow.
However, to even be able to implement these kinds of automations, payers first need to make their PA process electronic.
Ernst & Young estimates that even just digitization can significantly improve PA processes, bringing the time from submission to decision down to seven days for standard requests and 72 hours for expedited.
With the addition of automated PA triage, the CAQH estimates the entire healthcare industry could save $437 million a year from the benefits of digitized, near-real-time PA processes.
As we await movement from the government on possible regulation of PA algorithms, we urge impacted payers to familiarize themselves with how they may optimize their PA workflows—whether it’s sooner or later.
Building trust through data availability
Proposed CMS policy is forcing impacted payers to up their interoperability game, creating compliant FHIR APIs for patient, provider, and payers-to-payer access.
At the moment the interoperability ROI is simple: Compliance helps payers avoid penalties and negative payment adjustments. However, the financial opportunity does not end there.
Investment in FHIR APIs and associated data integration processes will also further reduce administrative friction for payers with respect to prior authorization. Seamless claims and encounter data flow will reduce time spent searching for relevant data and improve payers’ ability to meet regulatory requirements.

And in the end, giving providers greater access to real-time data—especially during transitions of care—helps reduce the utilization of high-cost care and increases the use of in-network providers. Plus, quick care gap identification boosts plan quality scores (such as MA Star ratings).
More than just meeting compliance thresholds, investing in interoperability builds goodwill in the broader healthcare ecosystem. As you seek to maintain a high-quality provider network and maintain a stellar reputation, your ability to “play nice” with the greater healthcare landscape will make your plans a more attractive choice.
Perhaps nothing will be more of a marker of this reputation than how well your patient and provider access APIs work. We recommend intentional investment in these data resources.
Takeaways: Teamwork for improved interoperability and prior authorization
Given our guidance on this page, we don’t recommend payers go about upgrading their PA and data-sharing processes and systems themselves. One of the best reasons to consult experts on these issues is that legacy system mindsets will hold you back from seeing the potential of strategic change.
Whether we’re building a comprehensive data strategy or mapping out how to align stakeholders through a period of organizational change, working with Curate Partners reduces time and headaches for payers in getting solutions like these operational.
Stay informed with our expertly curated healthcare updates. Sign up for our newsletter.



