Unlocking Efficiency:
A Guide to Automation Technologies for Healthcare Payers
Executive Summary:
There’s no way around it. The automation revolution has come for healthcare—and payers are no exception.
The more you look around, the fewer payers remain who haven’t implemented some form of AI-enabled automation in their business. These technologies are helping next-generation healthcare payers operate more efficiently and offer effortless white-glove service to their members and network.

However, much like healthcare, automation is not one-size-fits-all. Which automation technology you implement—and where in your business it fits best—is a very individual choice. To understand what automation upgrades would work best for your payer business, you need to feel confident with your knowledge of the automation landscape.
Whether you’re just getting started with automation for payers or looking to refine your toolkit, you’ve come to the right place.
At Curate Partners, we’ve worked with a range of payer organizations to refine a wide variety of business operations using automation. Now, we’re boiling down our automation experience for you, all in one accessible place. Consider this your crash course on the core automation technologies payers need to know.
The core automation technologies for payers:
- Robotic process automation (RPA)
- Smart workflows
- Computer vision
- Natural language processing (NLP)
- Cognitive agents
RPA for payers: Start your automation journey here
Robotic process automation (RPA) is one of the most powerful and relevant automation technologies for healthcare payers. It’s a game-changer for organizations seeking to streamline routine, rule-based tasks.
At a fundamental level, RPA works like this: Software robots mimic human interactions with digital systems. The result is a win-win—staff can redirect their attention to areas where their input is more necessary, and the business lowers their risk of administrative errors. Plus, because RPA relies on existing interfaces, implementing it doesn’t require a costly IT infrastructure overhaul.
In healthcare, RPA improves functions ranging from billing accuracy to regulatory compliance and credentialing. RPA can be so nimble because of how it can work with or without supervision. Attended RPA bots are activated by employees on workstations or private servers, giving organizations a high level of control over how the bot functions in collaboration. In comparison, unattended RPA bots ease automation at scale, working independently by relying on a preset schedule and meticulously constructed logic.
Expert estimates predict that up to 60 percent of the healthcare value chain can be automated with attended and unattended RPA.
McKinsey: Where machines could replace humans—and where they can’t (yet) UiPath: Robotic Process Automation (RPA) in the Healthcare Sector
UiPath also projects that automation with both attended and unattended bots gives healthcare organizations, on average, a 5.3-month ROI after a 5.2-week implementation time.
Supercharging claims processing with RPA
For healthcare payers, RPA can especially help speed up claims processing. Software robots can efficiently extract relevant information from incoming claims, validate data accuracy, and update records without human intervention. This accelerates the claims adjudication process and frees up human resources to focus on more complex tasks that require critical thinking and decision-making.
This accelerates the claims adjudication process and frees up human resources to focus on more complex tasks that require critical thinking and decision-making.
When paired with other automation—like smart workflows—payers can leverage RPA to significantly increase work intake while decreasing errors and adjudication time. For instance, a national U.S. payer saved $30 million in administrative costs while decreasing manual downstream processing. This further opened a door to digitizing 15 additional business operations.
From our experience, we’ve found RPA is the best place for payers interested in automation upgrades to start. We’ve worked with many payers implementing RPA across different business areas. If you’re wondering where RPA might improve your payer organization, we’d love to weigh in. Let’s start the automation conversation.
Smart workflows for payers: Creating integrated experiences
Imagine you’re a healthcare plan member. You’ve gotten used to having your digital health experiences operate like many of your favorite apps and lifestyle subscription services. Think sleek interfaces and seamless personalization. Why wouldn’t you expect your interactions with your health plan to be the same?
 Creating an elevated digital experience takes more than one step of automation. Don’t miss our specialized recommendations for digital transformation.
Creating an elevated digital experience takes more than one step of automation. Don’t miss our specialized recommendations for digital transformation.
One of the first steps toward creating that seamless digital experience is implementing smart workflows. Smart workflows leverage intelligent automation to streamline end-to-end processes.
As a payer, you can take advantage of smart workflows to optimize the entire healthcare management lifecycle—from member enrollment to claims processing. For instance, when a member submits a claim, a smart workflow can automatically trigger the necessary approvals, track the progress, and update stakeholders in real-time. Your overall member experience elevates with reduced processing times and increased transparency.
When it comes to updating business workflows, your payer business needs a rigorous and sensitive approach. That’s why our approach to change management pairs smart workflow design with stakeholder alignment and comprehensive change management education.
Computer vision: Leveraging payers’ unstructured data
 From our years of working with payer businesses, we understand that one of the biggest headaches is coordinating and integrating unstructured data.
From our years of working with payer businesses, we understand that one of the biggest headaches is coordinating and integrating unstructured data.
Healthcare as an industry manages so many forms of unstructured data—from discharge summaries to medical imaging. And that data is only growing. In fact, the rate of data generated across the industry has been rising at a rate of 47 percent per year.
Payers are no exception when it comes to the pains of handling all of that unstructured data. That unstructured data especially comes into play with document processing and fraud detection.
That’s where computer vision becomes a healthcare payer’s secret weapon.
If you’re already using this form of visual information processing automation, you’re likely using optical character recognition (OCR). This application of computer vision is most useful for tasks like verifying member identity documents. The days of manually inputting names from driver’s licenses are long behind us.
If you’re not yet using computer vision and OCR, now is the best time to get on board, as advances in artificial intelligence have made this automation technology much more accurate at pulling information from visual media.
And as natural language processing (NLP) techniques work with computer vision to improve OCR—especially when it comes to handwriting and lower image quality—the technology will continue to power how payers integrate unstructured data into their business operations.
NLP for enhanced healthcare payer communication

As we’ve covered, NLP pairs well with computer vision to help payers manage their unstructured data.
Of course, NLP is about more than powering the word-detection aspect of OCR.
NLP consists of the following automated tasks:
- Text classification
- Sentiment analysis
- Language translation
- Speech recognition
To put it most broadly: NLP is a form of AI that helps computers to interact with human language by breaking it down into its foundational parts.
Payers can take advantage of NLP to, for example, automate and error-proof diagnosis coding reviews and loop unstructured, free-text data into claims decision support.
In healthcare, organizations also use NLP to revolutionize how they communicate—with each other and with consumers. This is, of course, where generative AI chatbots come into play.
For payers, the customer-facing application of NLP is where we see the most momentum. An effective chatbot can lower the pressure on a payer’s customer service department by answering members’ common questions, guiding them through the enrollment process, or providing information on coverage options. After all, IBM has found that three out of four times, answers to customer service questions can be easily found on the company’s website. Even the most rudimentary NLP algorithm could remedy this source of waste.
Plus, when leveraging sentiment analysis, NLP could help payers better understand prospective and current members’ common frustrations, turning customer service into valuable customer experience (CX) research.
The result: A more focused customer service department and a more seamless, personalized digital experience for prospective and existing members alike.
Cognitive agents for personalized payer decision-making
As we’ve been mentioning, automation can be useful to organizations looking to dedicate their human resources to more critical evaluations. Even so, not every complex decision necessarily requires an entirely human touch.
 This is where cognitive agents come in. This automation technology bridges NLP with machine learning, creating virtual entities—agents—that perform tasks typically requiring human intelligence.
This is where cognitive agents come in. This automation technology bridges NLP with machine learning, creating virtual entities—agents—that perform tasks typically requiring human intelligence.
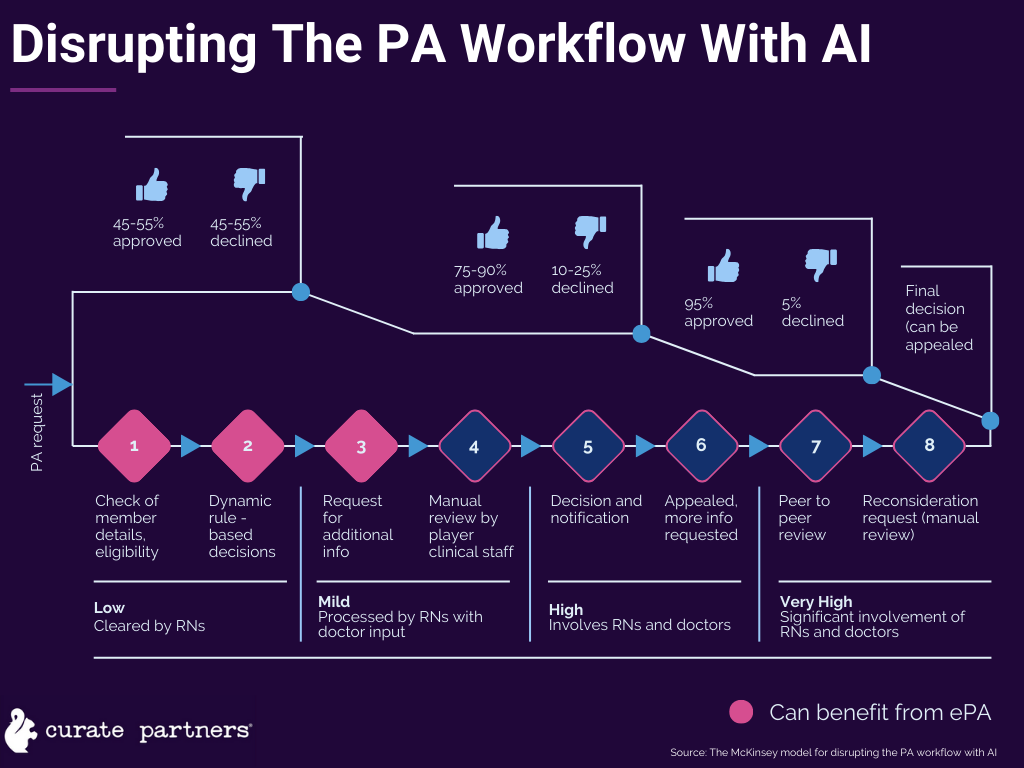
In healthcare, we commonly see this automation technology in AI-enabled clinical decision software. For healthcare payers, cognitive agents can especially come in handy for eligibility assessments and prior authorization.
Cognitive agents can analyze historical data, take into account the member’s medical history, and provide recommendations based on predefined eligibility criteria. Automating this process not only speeds up decision-making but also ensures that recommendations are consistent and aligned with clinical guidelines.
The difference in efficiency can be staggering. When Elevance Health began employing cognitive agents in its preauthorization processes, they were able to cut down urgent care authorizations from 72 hours to a few seconds. When it came to elective procedures, preauthorizations that previously took three to five days also came down to a few seconds with the cognitive technology.
Takeaways: How your payer business can get up to speed with automation technologies
The choice to automate processes in your payer business is a personal one. Your operation is unique in its mission, workflows, populations, and business plan.
The automation technology that is right for your business may not be what has brought other payers success. At the same time, with the rise of intelligent automation and advancements in AI, even the simplest of automation technologies—RPA—is growing further intertwined with the other core automation technologies. The most automation-savvy healthcare businesses are embracing this multi-faceted approach.
Overall, you must keep in mind that the journey toward greater automation is not just a technological upgrade—or a fad. It’s a strategic move aimed at keeping up and excelling in an increasingly digital and personalized healthcare landscape.
Embracing these automation technologies will not only drive operational excellence but also empower you to focus on your core mission of providing quality care to your members.
Let’s discuss how automation can future-proof your payer business. Get in touch.



