Leading the Way:
The Crucial Role of Executive Leadership in Payment Integrity
In the complex landscape of healthcare operations, one principle stands out above all: Payment Integrity (PI) starts at the top. At the helm of every successful PI initiative lies the unwavering commitment and strategic vision of executive leadership. As highlighted in a recent article, “10 Lessons Learned While Implementing a Payment Integrity Office,” the journey towards PI excellence is paved with valuable insights and lessons. Here’s why executive buy-in is not just essential but indispensable in driving Payment Integrity within healthcare finance.

1. Developing an Effective PI Organization:
Executive leadership serves as the catalyst for developing a robust PI organization. Their guidance and direction are pivotal in shaping the ongoing structure, policies, and objectives necessary to ensure long term financial stewardship.
2. Fostering Collaboration Across the Organization:
3. Embracing Provider Abrasion:
Explore our Payment Integrity Program Implementation Solutions
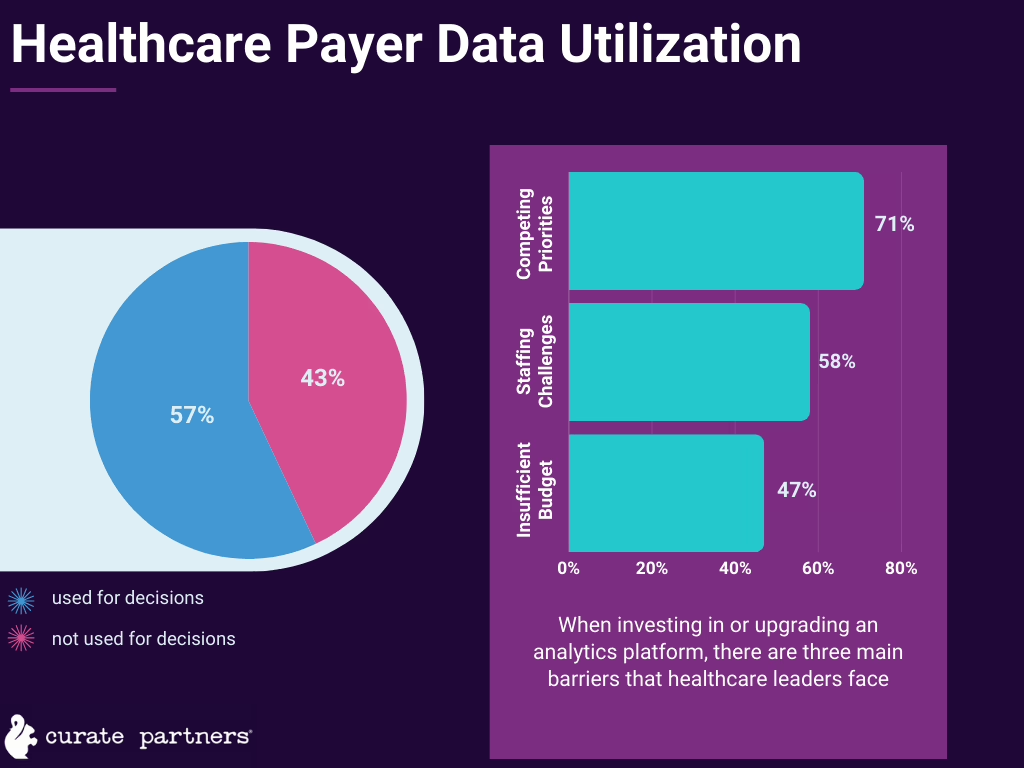
4. Investing in Resources and Tools:
5. Recognizing Pre-Payment Savings:

Conclusion:
In conclusion, executive leadership plays a pivotal role in driving Payment Integrity within healthcare operations and finance. Their vision, commitment, and strategic direction are indispensable in fostering collaboration, embracing challenges, and ultimately, ensuring the financial well-being and ongoing support of the organization.



















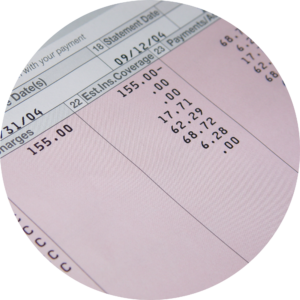 Another challenge in maintaining payment integrity is the occurrence of billing errors and inaccurate claims. These errors can arise due to coding mistakes, documentation discrepancies, or misunderstandings of reimbursement guidelines. Inaccurate claims can result in overpayment or underpayment of healthcare providers, leading to financial inaccuracies and disputes.
Another challenge in maintaining payment integrity is the occurrence of billing errors and inaccurate claims. These errors can arise due to coding mistakes, documentation discrepancies, or misunderstandings of reimbursement guidelines. Inaccurate claims can result in overpayment or underpayment of healthcare providers, leading to financial inaccuracies and disputes.